So you’ve probably heard of Medicaid and Medicare, right? These are two government programs in the United States that provide healthcare coverage for certain individuals and groups. But did you know that these programs also cover air ambulance services? That’s right! If you’re in need of emergency medical transportation via air, Medicaid and Medicare can help ease the financial burden. In this article, we’ll take a closer look at how these programs provide coverage for air ambulance services and what you need to know if you ever find yourself in a situation where you need this type of assistance. So sit back, relax, and let’s explore the world of Medicaid and Medicare coverage for air ambulance services!

What is Medicaid?
Medicaid is a joint federal and state program that provides healthcare coverage to low-income individuals and families who meet certain eligibility criteria. It is designed to assist those who cannot afford private health insurance or have limited access to employer-sponsored coverage. Medicaid is administered by states, and each state has its own set of rules and requirements for enrollment.
Definition of Medicaid
Medicaid is a government-funded program that offers medical assistance to people with low income and limited resources. It provides a range of healthcare services, including doctor visits, hospital stays, prescription medications, and preventive care. Medicaid plays a crucial role in ensuring that individuals and families have access to necessary healthcare services, regardless of their financial situation.
Medicaid Eligibility
To qualify for Medicaid, you must meet certain eligibility criteria, which vary by state. Generally, Medicaid is available to low-income individuals, pregnant women, children, and individuals with disabilities. Eligibility is primarily based on income and household size, with the program targeting those with the greatest need. Each state has different income thresholds and asset limits, so it’s important to check your state’s specific requirements.
Covered Services Under Medicaid
Medicaid provides a wide range of covered services, including doctor visits, hospital care, laboratory tests, mental health services, and medications. Additionally, it covers preventive care such as vaccinations, cancer screenings, and family planning services. Some states also offer additional benefits like dental and vision care. It’s crucial to familiarize yourself with your state’s Medicaid program and the specific services covered to ensure you receive the care you need.
What is Medicare?
Medicare is a federal health insurance program primarily for individuals aged 65 and older, as well as certain younger individuals with disabilities. It consists of different parts that cover specific healthcare services. Medicare is administered by the Centers for Medicare & Medicaid Services (CMS) and provides healthcare coverage to over 60 million Americans.
Definition of Medicare
Medicare is a government-run health insurance program that provides coverage to eligible individuals, including seniors and individuals with disabilities. It is divided into several parts, each covering different types of healthcare services. Medicare helps ensure that older adults and those with disabilities have access to essential healthcare services, allowing them to lead healthier lives.
Medicare Eligibility
To be eligible for Medicare, you must meet certain requirements. Generally, individuals aged 65 and older are eligible, as well as individuals under 65 with certain disabilities or end-stage renal disease. Most people become eligible for Medicare automatically when they turn 65, but there are specific enrollment periods and requirements that vary based on individual circumstances. It’s essential to understand your eligibility and enroll in the appropriate parts of Medicare.
Covered Services Under Medicare
Medicare offers coverage for various healthcare services, including hospital stays, doctor visits, preventive care, and prescription medications. It consists of different parts, such as Part A (hospital insurance), Part B (medical insurance), Part C (Medicare Advantage), and Part D (prescription drug coverage). Each part covers different services, and individuals can choose the coverage options that best meet their needs.
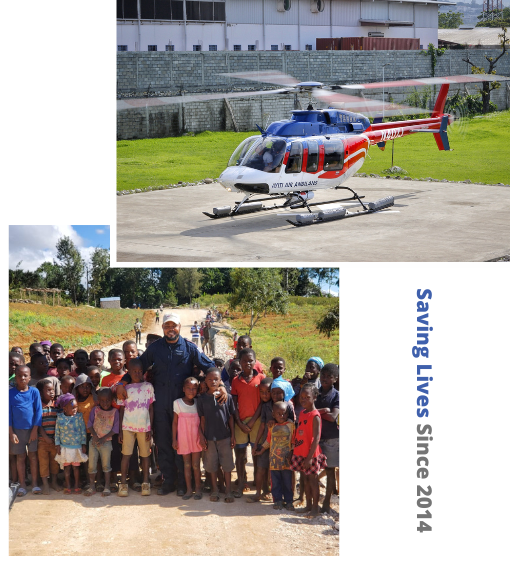
Air Ambulance Services
Air ambulance services are specialized medical transport services that utilize aircraft, such as helicopters or fixed-wing planes, to transport patients in need of critical care over long distances or in emergency situations. These services are typically staffed by skilled medical professionals, including doctors and nurses, who can provide advanced medical care during the transportation.
Understanding Air Ambulance Services
Air ambulance services are an essential component of the healthcare system, as they play a vital role in transporting patients who require immediate medical attention. These services are particularly crucial in rural areas with limited access to specialized medical facilities. Air ambulances are equipped with advanced medical equipment and can efficiently transport patients to the nearest appropriate healthcare facility, ensuring timely and lifesaving interventions.
When Are Air Ambulances Necessary?
Air ambulances are necessary when ground transportation is not feasible or appropriate due to the patient’s critical condition or the distance involved. They are commonly used in emergency situations, such as severe trauma, cardiac events, or complications during childbirth. Additionally, air ambulances may be utilized for non-emergency cases when time-sensitive specialized medical care is required, such as organ transplants or accessing specialized healthcare facilities.
Benefits of Air Ambulance Services
Air ambulance services offer several benefits that can potentially save lives and improve patient outcomes. The speed and efficiency of air transportation allow patients to reach specialized medical facilities quickly, reducing the time it takes to receive critical care. Moreover, air ambulances provide a controlled and monitored environment, ensuring that patients receive consistent medical attention throughout the journey. This level of care can make a significant difference, especially for patients with critical conditions or those in need of specialized procedures.
Medicaid Coverage for Air Ambulance Services
Medicaid provides coverage for air ambulance services under certain circumstances, ensuring that eligible individuals receive the necessary transport to receive appropriate medical care. However, it’s important to understand the coverage criteria, reimbursement rates, and any limitations or restrictions that may apply.
Medicaid Coverage Criteria for Air Ambulance Services
Medicaid generally covers air ambulance services when they are medically necessary and deemed the most appropriate means of transportation. The eligibility for coverage varies by state, and each state may have specific requirements that must be met. It is typically necessary to have a referring healthcare provider who certifies the need for air transportation.
Reimbursement Rates for Air Ambulance Services
The reimbursement rates for air ambulance services under Medicaid can vary depending on the state and the specific circumstances. Medicaid typically pays for a portion of the service cost, and the exact reimbursement rate may depend on factors such as the distance traveled, the level of care provided, and the state’s fee schedule. It’s important to consult your state’s Medicaid program for specific information on reimbursement rates.
Limitations and Restrictions
Medicaid coverage for air ambulance services may be subject to limitations and restrictions. These can include restrictions on the types of medical conditions that qualify for air transportation, geographical limitations, and documentation requirements. It’s important to thoroughly understand your state’s Medicaid rules and guidelines to ensure you meet all necessary criteria for coverage.

Medicare Coverage for Air Ambulance Services
Medicare also offers coverage for air ambulance services when certain criteria are met. Medicare beneficiaries can access air transportation for emergency situations or when ground transportation is not feasible or appropriate. However, it’s important to understand the coverage criteria, reimbursement rates, and any limitations or restrictions that may apply.
Medicare Coverage Criteria for Air Ambulance Services
Medicare coverage for air ambulance services is generally based on medical necessity. It covers transportation when a patient’s condition is such that ground transportation would endanger their health or when the nearest appropriate medical facility is unreasonably far. Medicare requires the use of the closest appropriate facility and may not cover air transportation to specialized hospitals or facilities if a closer alternative is available.
Reimbursement Rates for Air Ambulance Services
Medicare reimbursement rates for air ambulance services vary depending on the specific circumstances and the Geographic Statistical Area (GSA) in which the service is provided. Medicare has established fee schedules and reimbursement formulas to determine the amount paid for air ambulance transportation. The reimbursement rates may not cover the full cost of the service, and patients may be responsible for any remaining balance.
Limitations and Restrictions
Medicare coverage for air ambulance services is subject to limitations and restrictions. These can include requirements for medical certification, limitations on the use of specialized hospitals, and documentation requirements. Medicare also does not cover air transportation for non-emergency purposes or when ground transportation is feasible and appropriate. Understanding the specific guidelines and requirements is essential to ensure coverage eligibility.
Difference Between Medicaid and Medicare Coverage
While both Medicaid and Medicare provide healthcare coverage, there are significant differences between the two programs, particularly regarding eligibility, covered services, and reimbursement rates.
Differences in Eligibility
Medicaid primarily targets low-income individuals and families, including pregnant women, children, and individuals with disabilities. Eligibility is based on income and household size, and specific requirements vary by state. On the other hand, Medicare is available to individuals aged 65 and older, as well as those with certain disabilities, regardless of income.
Differences in Covered Services
Medicaid covers a broad range of healthcare services, including doctor visits, hospital care, prescription medications, and preventive care. The specific services covered may vary by state. Medicare, on the other hand, consists of different parts that cover specific healthcare services, such as hospital stays, doctor visits, prescription drug coverage, and additional benefits available through Medicare Advantage plans.
Differences in Reimbursement Rates
Medicaid and Medicare have different reimbursement rates for healthcare services, including air ambulance transportation. Medicaid reimbursement rates vary by state, and the rates may not cover the full cost of the services provided. Medicare has established fee schedules and reimbursement formulas that determine the amount paid for specific services, including air ambulance transportation.
Factors Affecting Coverage
Several factors can influence coverage for air ambulance services, regardless of whether you have Medicaid or Medicare. These factors include medical necessity, distance of transport, and the availability of ground transportation alternatives.
Medical Necessity
Both Medicaid and Medicare require that air ambulance services be deemed medically necessary for coverage. This means that the patient’s condition must genuinely necessitate air transportation due to the critical nature of their illness or injury. Medical providers play a crucial role in determining and certifying medical necessity.
Distance of Transport
The distance that needs to be covered plays a significant role in determining whether air ambulance services are necessary. Long distances or remote locations where ground transportation would take too long or pose a risk to the patient’s health increase the likelihood of air ambulance coverage.
Availability of Ground Transportation
The availability and accessibility of ground transportation alternatives also impact the coverage for air ambulance services. If an appropriate medical facility can be reached within a reasonable time and distance using ground transportation, coverage for air ambulance services may be denied.
How to Utilize Medicaid and Medicare Coverage
Understanding how to effectively utilize Medicaid and Medicare coverage for air ambulance services is essential to avoid potential challenges and ensure necessary care is received.
Understanding the Process
Familiarize yourself with the specific guidelines and requirements of your state’s Medicaid program or Medicare coverage for air ambulance services. Be aware of the necessary documentation, medical certification, and any pre-approval processes that may be required.
Getting Pre-Approval
In some cases, pre-approval or prior authorization may be required for air ambulance services to be covered. Check with your Medicaid or Medicare provider to determine if pre-approval is necessary and follow the specified process to obtain it, if applicable.
Filing Insurance Claims
Once air ambulance services have been provided, it’s important to properly file insurance claims with your Medicaid or Medicare provider. Ensure that all necessary documentation is included and that the claim is submitted within the specified timeframes. Be prepared to provide any additional information or documentation that may be requested.
Appealing Coverage Denials
Coverage denials for air ambulance services can occur, but it’s important to know that there are steps you can take to appeal these decisions.
Steps to Appeal a Coverage Denial
If your Medicaid or Medicare provider denies coverage for air ambulance services, you have the right to appeal the decision. This typically involves writing a letter outlining the reasons for the appeal and providing any supporting documentation that may strengthen your case.
Gathering Necessary Documentation
When appealing a coverage denial, gather all relevant documentation to support your claim. This can include medical records, the opinion of a healthcare professional, and any other pertinent evidence that demonstrates the medical necessity and appropriateness of air ambulance services in your situation.
Seeking Assistance or Legal Advice
If you face challenges or complexities during the appeals process, consider seeking assistance or legal advice. There are organizations and professionals who specialize in healthcare advocacy and can provide guidance and support to ensure your rights are protected.
Other Financing Options
In addition to Medicaid and Medicare coverage, there may be other financing options available to help cover the cost of air ambulance services.
Charitable Organizations
Certain charitable organizations offer financial assistance or grants to individuals in need of air ambulance services. These organizations may have specific eligibility criteria or requirements, so it’s important to research and reach out for potential assistance.
Private Insurance
If you have private health insurance, it may provide coverage for air ambulance services. Review your insurance policy and contact your insurance provider to understand the specific coverage options and any limitations or restrictions that may apply.
Personal Payment Arrangements
If no other financing options are available or feasible, personal payment arrangements may need to be considered. Air ambulance services can be costly, so it’s essential to discuss payment options and potential financial assistance with the air ambulance provider to make suitable arrangements.
In conclusion, understanding the coverage provided by Medicaid and Medicare for air ambulance services is crucial for individuals who may require emergency or critical care transportation. Being knowledgeable about eligibility criteria, covered services, reimbursement rates, and potential limitations or restrictions can empower individuals to navigate these healthcare programs effectively. Additionally, awareness of the factors affecting coverage, tips on utilizing coverage, and potential financing options can help individuals overcome challenges and access the necessary care they need in times of medical emergencies.