Hey there! In this article, we’re going to tackle a topic that’s often overlooked but incredibly important: air ambulance billing transparency. If you or a loved one has ever needed air ambulance services, you know that it can be an expensive endeavor. But what many patients don’t realize is that navigating the world of air ambulance billing can be just as challenging as the medical emergency itself. So, we’re here to shed some light on what patients should know when it comes to understanding and navigating the complex world of air ambulance billing. Buckle up, because we’re diving deep into this topic to ensure you have all the information you need.
Why Air Ambulance Billing Transparency is Important
If you or a loved one has ever needed air ambulance services, you know just how stressful and overwhelming the experience can be. Not only are you dealing with a medical emergency, but you’re also faced with the daunting task of understanding and navigating the complex world of air ambulance billing. This is where the importance of air ambulance billing transparency comes into play.
Understanding the Importance of Air Ambulance Billing Transparency
Billing transparency is crucial in the air ambulance industry because it empowers patients to make informed decisions about their medical care and financial responsibilities. When patients have access to clear and detailed information about the cost of air ambulance services, they can better anticipate and plan for the financial impact of such critical transportation.
Additionally, transparency in billing practices allows patients to hold air ambulance providers accountable for their pricing and billing methods. By shedding light on the often convoluted and confusing billing process, patients can advocate for fair and reasonable charges, and avoid being taken advantage of by surprise billing practices.
The Impact of Non-transparent Billing Practices on Patients
Non-transparent billing practices in the air ambulance industry can have significant negative consequences for patients. One of the most prominent issues is the prevalence of surprise billing, where patients receive unexpectedly high bills for air ambulance services that their insurance provider refuses to fully cover.
This lack of transparency creates a tremendous financial burden on patients and their families during an already challenging time. In some cases, patients may be forced to choose between paying exorbitant medical bills or forgoing necessary medical treatment altogether. These financial hardships can have long-lasting consequences on individuals and families, leading to medical debt and financial instability.
Potential Benefits of Increased Billing Transparency
Increasing billing transparency in the air ambulance industry can bring about several benefits for patients. First and foremost, it helps patients understand the cost of air ambulance services and allows them to budget and plan accordingly. By knowing what to expect, patients can seek out insurance coverage that best meets their needs and explore alternative options, if available.
Moreover, increased transparency can foster competition among air ambulance providers, leading to more cost-effective services. When providers are held accountable for their pricing and billing practices, they are more likely to offer fair rates and provide better value for patients. Ultimately, this can lead to a more efficient and patient-centric air ambulance industry.
Air Ambulance Billing Process
Understanding the intricacies of the air ambulance billing process is essential for patients to navigate the often confusing and overwhelming world of medical bills. By gaining insight into how billing works, patients can better advocate for themselves and make informed decisions about their medical and financial choices.
An Overview of the Air Ambulance Billing Process
The air ambulance billing process typically begins with the provider gathering essential information about the patient, such as their insurance coverage, medical needs, and the nature of the transport. This information helps determine the appropriate billing codes and establishes the basis for the charges.
Once the transport has taken place, the air ambulance provider generates an itemized bill that includes various components, such as aircraft usage, medical personnel, equipment, medications, and any additional services provided. This bill is then submitted to the patient’s insurance company for review and payment.
The Role of Insurance in Air Ambulance Billing
Insurance coverage plays a significant role in air ambulance billing. Depending on the patient’s insurance plan and provider network, the air ambulance transport may be considered either in-network or out-of-network. In-network providers have negotiated contracts with certain insurance companies, which often result in lower costs for the patient. Out-of-network providers, on the other hand, do not have negotiated contracts and may charge higher rates.
It is crucial for patients to understand their insurance coverage and any limitations or exclusions related to air ambulance services. This knowledge can help patients anticipate their out-of-pocket costs and make informed decisions about seeking care from in-network providers whenever possible.

Common Components of Air Ambulance Bills
Air ambulance bills typically include various components that contribute to the overall cost of the transport. These components can vary depending on the specific circumstances of the transport and the provider’s billing practices. Some common components found in air ambulance bills include:
- Base rate: This is the basic charge for the use of the air ambulance, which includes the cost of the aircraft itself and related operational expenses.
- Medical personnel: Air ambulance bills may include charges for the medical personnel involved in the transport, such as doctors, nurses, and paramedics.
- Equipment and supplies: The use of specialized equipment, medical supplies, and medications during the transport can also contribute to the overall cost of air ambulance services.
- Ground transportation: In certain cases, ground transportation may be necessary to transport the patient to and from the air ambulance. These costs may also be included in the bill.
- Communication and coordination: Air ambulance providers often incur costs related to communication and coordination with medical facilities, insurance companies, and other involved parties. These costs may also be reflected in the bill.
It is important for patients to carefully review their air ambulance bills and seek clarification from the provider about any charges that are unclear or seem excessive. Understanding the breakdown of charges can help patients identify any potential errors or billing discrepancies.
Factors Affecting Air Ambulance Costs
The cost of air ambulance services can vary significantly depending on several factors. Understanding these factors can help patients anticipate and better comprehend the pricing associated with air ambulance transports.
Distance and Geographical Considerations
One of the primary factors impacting air ambulance costs is the distance of the transport and the geographical location involved. Longer distances and remote locations often require more fuel, increased flight time, and additional logistical challenges, all of which can contribute to higher costs.
Air ambulance providers must consider these factors when determining their pricing structure. Patients should be aware that transports involving longer distances or remote areas are likely to be more expensive than those within shorter distances or more populated regions.
Aircraft Type and Equipment
The type of aircraft and the necessary equipment for the transport can also affect air ambulance costs. Different aircraft have varying capacities, capabilities, and fuel efficiencies, which can influence pricing. Helicopters, for example, are generally more expensive to operate than fixed-wing aircraft, due to their smaller size and shorter range.
Additionally, the equipment required for a specific medical condition or situation can impact the overall cost. Specialized medical equipment, such as ventilators, cardiac monitors, or neonatal incubators, may be necessary for certain patients, and the inclusion of such equipment can lead to higher costs.
Medical Staff and Services
The medical personnel involved in an air ambulance transport, as well as any additional medical services provided, can contribute to the overall cost. Highly trained and experienced doctors, nurses, and paramedics form an essential part of the air ambulance team, ensuring the highest level of care during the transport.
Furthermore, some air ambulance providers may offer additional services, such as specialized medical consultations, telemedicine support, or advanced life support capabilities. These additional services, while valuable, may also result in higher costs for the patient.
Additional Factors Influencing Air Ambulance Costs
There are other factors beyond distance, aircraft type, and medical staff that can influence air ambulance costs. These include:
- Time of transport: Transports during peak hours or at night may incur higher costs due to increased demand or the need for additional staffing.
- Weather conditions: Adverse weather conditions can affect the suitability and safety of air ambulance flights. Delays or diversions caused by weather can result in additional costs.
- Ground support and landing fees: Depending on the specific location and infrastructure, air ambulance providers may have to pay landing fees or require ground support services, which can contribute to the overall cost.
- Administrative and operational expenses: Air ambulance companies incur administrative and operational costs, such as maintaining aircraft, licensing and certifications, insurance, and staffing, which are factored into the price of the service.
Patients should be aware that these additional factors can influence the final cost of air ambulance services. Understanding the various factors that affect pricing can help patients make more informed decisions and better anticipate their financial responsibilities.
Common Billing Practices in the Air Ambulance Industry
In the air ambulance industry, several billing practices can significantly impact patients and their financial well-being. Understanding these common practices is crucial for patients to navigate the complexities of air ambulance billing.

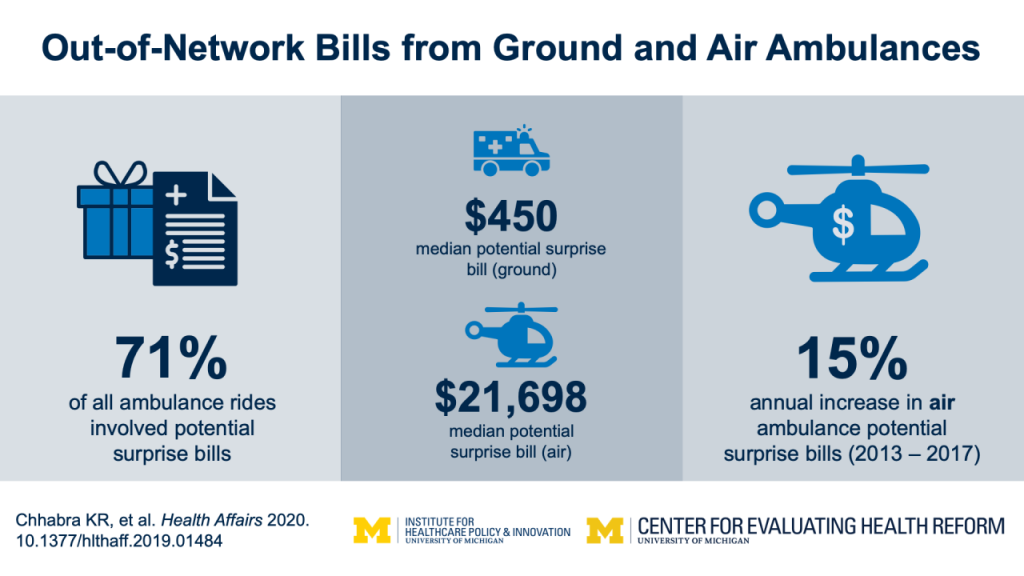
The Prevalence of Surprise Billing
Surprise billing, also known as balance billing, is a widespread issue in the air ambulance industry. Surprise billing occurs when patients receive unexpectedly high bills for air ambulance services that their insurance provider refuses to fully cover.
In many cases, air ambulance providers are considered out-of-network for insurance purposes. This means that they do not have negotiated contracts with insurance companies, allowing them to charge higher rates. As a result, patients may be left with substantial out-of-pocket expenses, as their insurance provider may only cover a portion of the charges.
Surprise billing can impose a significant financial burden on patients, who may be caught off guard by the unexpectedly high costs. It is important for patients to be aware of this practice and understand their insurance coverage to avoid being blindsided by substantial bills.
In-Network and Out-of-Network Providers
The distinction between in-network and out-of-network providers is essential when it comes to air ambulance billing. In-network providers have negotiated contracts with certain insurance companies, resulting in lower costs for patients. These contracts typically set predetermined rates for services and establish agreed-upon payment structures.
Out-of-network providers, on the other hand, do not have negotiated contracts with specific insurance companies. This means they can charge higher rates, potentially leaving patients responsible for a more significant portion of the bill.
Patients should familiarize themselves with their insurance plan and determine whether their air ambulance provider is considered in-network or out-of-network. This knowledge can help patients anticipate their out-of-pocket costs and make informed decisions about accessing care from in-network providers whenever possible.
Balance Billing and Its Impact on Patients
Balance billing is a practice that occurs when an air ambulance provider bills the patient for the difference between their charges and the amount insurance covers. This occurs when the provider is an out-of-network provider or when the insurance company determines that the charges exceed what they consider to be reasonable and customary.
For example, if an air ambulance provider charges $50,000 for a transport and the insurance company determines that the reasonable and customary cost is $30,000, the patient may be left responsible for the remaining $20,000. This unexpected additional expense can place a significant financial burden on patients, especially in situations where they have no control over the choice of provider.
Balance billing is a contentious issue and has garnered increased attention in recent years. Efforts to address this practice aim to protect patients from exorbitant billing charges and ensure they are not placed under undue financial stress when seeking critical air ambulance services.
The Payer’s Role in Determining Patient Costs
Insurance companies play a vital role in determining the cost responsibility of the patient for air ambulance services. The specific terms of a patient’s insurance plan, such as deductibles, co-pays, and out-of-pocket maximums, can significantly impact the amount the patient will be responsible for paying.
It is important for patients to thoroughly review their insurance policy and understand their financial obligations. Additionally, patients should consider discussing their coverage with their insurance provider directly to gain clarity on what expenses they can expect to incur for air ambulance services.
By understanding the payer’s role in determining patient costs, individuals can better advocate for themselves and make more informed decisions regarding their medical care and finances.
The Importance of Prior Authorization
Prior authorization is a critical aspect of the air ambulance billing process that both patients and providers need to understand. By being familiar with the concept and requirements of prior authorization, patients can mitigate potential billing issues and ensure smoother interactions with their insurance companies.
Understanding the Concept of Prior Authorization
Prior authorization refers to the process where the patient’s insurance provider must approve and authorize specific medical services before they are performed. In the context of air ambulance transportation, prior authorization serves as a safeguard for both the patient and the insurer.
By requiring prior authorization, insurance companies can assess the medical necessity of air ambulance services and effectively manage costs. This process helps prevent unnecessary or inappropriate use of air ambulance resources, ensuring that they are reserved for cases where ground transportation is not feasible or could result in significant harm to the patient.

How Prior Authorization Affects Air Ambulance Billing
The absence of prior authorization for air ambulance services can lead to significant challenges in the billing process. Insurance companies may consider transports without prior authorization to be non-emergency or not medically necessary, which can result in a denial of coverage or reduced reimbursement.
Without prior authorization, patients may be left responsible for the entirety of the air ambulance bill, placing them at substantial financial risk. It is imperative for patients to understand the importance of prior authorization and work closely with their medical providers to ensure all necessary steps are taken to obtain approval from their insurance company.
Potential Challenges and Solutions
The prior authorization process can present challenges for patients, as it often requires coordination and communication between various parties, including medical providers, insurance companies, and patients themselves. Delays in obtaining prior authorization can result in delayed or denied coverage, creating additional stress and financial burdens for patients.
To navigate these challenges effectively, patients can take proactive steps to streamline the prior authorization process. This includes providing the necessary medical documentation, promptly submitting prior authorization requests, and following up with insurance companies to ensure timely approval.
It is also beneficial for patients to familiarize themselves with their insurance company’s prior authorization requirements and policies. Understanding the specific criteria used to determine medical necessity can better equip patients to provide the necessary evidence to support their case.
Ultimately, prioritizing prior authorization is essential for patients to receive adequate insurance coverage for air ambulance services. By working closely with medical providers and insurance companies, patients can minimize potential billing issues and ensure a smoother process for all parties involved.
Transparency Efforts and Regulation
Recognizing the need for improved air ambulance billing transparency, various stakeholders have initiated efforts to address the issue. These efforts aim to enhance patient understanding, promote fair billing practices, and hold air ambulance providers accountable. Both state and federal regulations play a significant role in driving these transparency initiatives.
Current Efforts to Improve Air Ambulance Billing Transparency
Several organizations, advocacy groups, and governmental bodies are actively working towards improving air ambulance billing transparency.
Non-profit organizations like the Air Patient Advocate Network (APAN) and Patient AirLift Services (PALS) focus on advocating for patients’ rights and providing support in navigating the air ambulance industry. These organizations work to raise awareness about the challenges patients face and promote transparency in billing practices.
On a governmental level, the Centers for Medicare and Medicaid Services (CMS) have taken steps to address air ambulance billing issues. The CMS has proposed regulations that require air ambulance providers to provide cost estimates to patients and establish clearer billing practices. These regulations aim to empower patients by providing them with essential information regarding their financial responsibilities upfront.
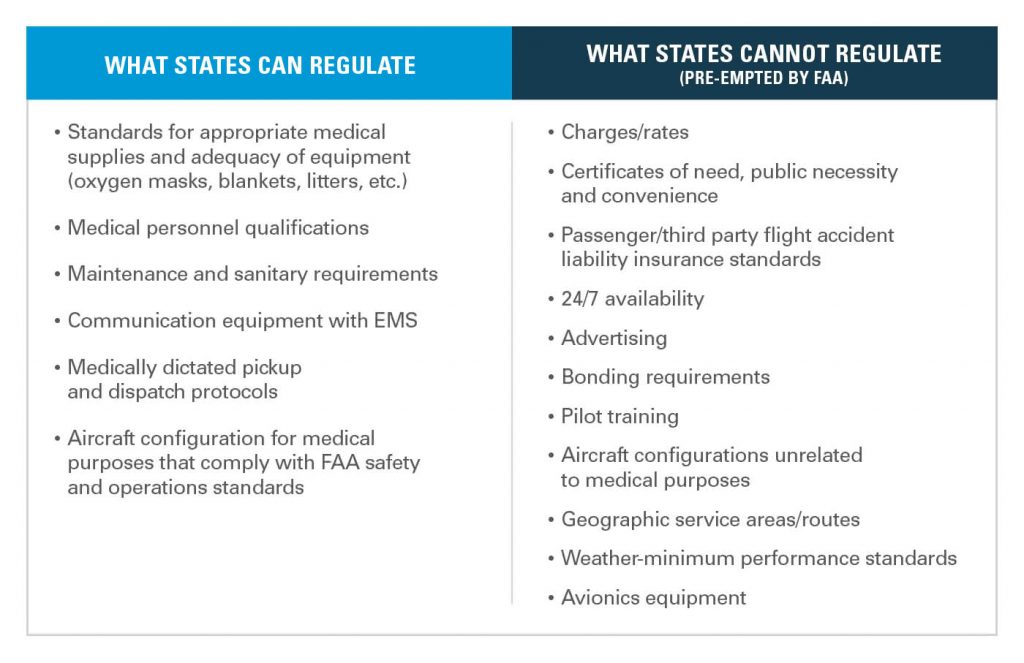
The Role of State and Federal Regulations
Both state and federal regulations play a vital role in shaping the air ambulance industry and addressing billing transparency.
At the state level, many states have implemented or are considering legislation to protect consumers from surprise billing and promote fair pricing in the air ambulance sector. These regulations often focus on improving transparency by requiring air ambulance providers to disclose pricing information and establishing guidelines for out-of-network billing.
On the federal level, there have been discussions about potential legislation aimed at addressing air ambulance billing practices. These proposals focus on establishing reasonable rates, ensuring adequate insurance coverage, and protecting patients from excessive charges.
Federal and state regulations work together to create a framework that encourages air ambulance providers to be more transparent in their billing practices, while also protecting patients from financial hardships.
The Impact of Regulatory Changes on Patients
Regulatory changes have the potential to significantly impact patients who require air ambulance services. Improved billing transparency, fairer pricing, and protection against surprise billing can alleviate the financial burden on patients and improve their overall experience within the air ambulance industry.
When air ambulance providers are required to provide clear and detailed cost estimates before transport, patients can make more informed decisions and plan for their financial responsibilities. Furthermore, regulations that establish reasonable rates and promote fair billing practices can protect patients from excessive charges and help prevent financial hardship.
However, it is essential to strike a balance between patient protection and the financial viability of air ambulance providers. Excessive regulation may inadvertently lead to reduced access to air ambulance services or hinder the industry’s ability to maintain high standards of care. Therefore, it is crucial for regulators to consider multiple perspectives and collaborate with stakeholders to develop sustainable solutions that prioritize patient well-being and maintain the availability of critical air transportation.
Steps Patients Can Take to Navigate Air Ambulance Billing
While the air ambulance billing process may seem overwhelming, there are steps that patients can take to navigate this complex landscape and advocate for fair and reasonable charges. By understanding their rights, seeking assistance, and proactively managing their medical bills, patients can better control their financial outcomes.
Seeking and Clarifying Insurance Coverage
One of the first steps patients should take is to thoroughly review their insurance coverage and understand what air ambulance services are included and to what extent. This includes determining whether their insurance provider considers the air ambulance provider to be in-network or out-of-network.
If there are any uncertainties or ambiguities regarding coverage, patients should contact their insurance company directly to seek clarification. It is essential to document all conversations and maintain records of communication with the insurance company for future reference.
Understanding and Negotiating Medical Bills
Upon receiving an air ambulance bill, patients should carefully review the itemized charges and seek clarification from the provider regarding any unclear or excessive charges. Patients have the right to understand what they are being billed for and should not hesitate to question any items that seem unreasonable or erroneous.
If the charges appear excessive or unfair, patients can consider negotiating with the air ambulance provider. Many providers are willing to work with patients to establish mutually agreeable payment plans or even potentially reduce the total amount owed.
It may also be beneficial for patients to consult with a healthcare billing advocate or medical billing specialist who can provide guidance and support in navigating the negotiation process.
Appealing Unexpected Charges
In cases where patients receive surprise bills or are balance billed for air ambulance services, it is important for them to understand their rights and options. Patients have the right to appeal unfair charges and file a complaint with their state insurance department if necessary.
Patients should gather all relevant documentation, including medical records, insurance policy information, and correspondence from the air ambulance provider, to support their appeal. It may be beneficial to seek the assistance of a healthcare billing advocate or legal counsel experienced in medical billing disputes to ensure a well-prepared and effective appeal.
Utilizing Consumer Protection Agencies and Resources
In addition to seeking assistance from healthcare billing advocates, patients can also utilize various consumer protection agencies and resources to help navigate the air ambulance billing process.
State insurance departments are valuable resources for patients seeking guidance and support in dealing with unfair billing practices. These departments can provide information on state-specific regulations, assist in filing complaints, and help mediate disputes between patients and insurance providers.
Additionally, national organizations like the Consumer Financial Protection Bureau (CFPB) and the Federal Trade Commission (FTC) offer resources and educational materials on healthcare billing and consumer rights. By familiarizing themselves with the available resources, patients can better arm themselves with the information necessary to protect their interests.
Advocacy for Improved Air Ambulance Billing Practices
Patients and advocacy groups play a crucial role in driving change and pushing for improved air ambulance billing practices. By uniting their voices and advocating for fair and transparent billing, they can influence legislation and policies that protect patients’ rights and promote affordability.
Supporting Organizations and Advocacy Groups
There are numerous organizations and advocacy groups dedicated to supporting patients and working towards fairer air ambulance billing practices. These organizations focus on raising awareness, providing resources, and advocating for legislative changes that benefit patients.
Groups like the Association of Air Medical Services (AAMS), Air Ambulance Association of America (AAAA), and Families for Air Ambulance Equity (FAAE) actively work towards protecting patients from excessive billing charges and promoting greater transparency in the industry. These organizations provide valuable information, resources, and support for patients navigating the air ambulance billing process.
Campaigning for Legislative Changes
To address the challenges posed by air ambulance billing, patients and advocacy groups can actively campaign for legislative changes at both state and federal levels. By sharing personal stories, contacting legislators, and participating in public awareness campaigns, advocates can raise awareness and influence lawmakers to prioritize fair and transparent billing practices.
Campaigns for legislative changes may include urging lawmakers to establish rate regulations, improve insurance coverage for air ambulance services, and enforce greater transparency in billing practices. Additionally, advocates can support reforms that protect patients from surprise billing and establish guidelines for appropriate reimbursement.
Engaging in Public Awareness and Education
Promoting public awareness and education is a powerful tool for advocates seeking improved air ambulance billing practices. By sharing information, personal experiences, and resources, advocates can empower patients to become informed consumers and make smarter decisions regarding their medical care and finances.
Advocates can engage in various initiatives to raise awareness, such as organizing community events, creating online resources and educational materials, and collaborating with local media outlets to disseminate information. By reaching a broader audience, advocates can foster a public conversation about the importance of fair medical billing and encourage individuals to be proactive in advocating for themselves.
Questions Patients Should Ask
To further help patients navigate the complexities of air ambulance billing, it is crucial for them to ask the right questions and gather the necessary information to make informed decisions.
What Factors Determine Air Ambulance Costs?
Patients should inquire about the specific factors that contribute to the overall cost of air ambulance services. Understanding how distance, aircraft type, medical staff, and additional factors influence pricing can enable patients to anticipate costs and make more informed decisions.
Is the Air Ambulance Provider In-Network or Out-of-Network?
Patients should be aware of whether the air ambulance provider they are considering is considered in-network or out-of-network by their insurance policy. This knowledge can help patients understand potential cost differences and seek care from in-network providers whenever possible.
What Does My Insurance Cover and What Are My Out-of-Pocket Costs?
Understanding the extent of insurance coverage for air ambulance services is crucial. Patients should ask their insurance provider for a detailed explanation of coverage, deductibles, co-pays, and any other out-of-pocket expenses they may be responsible for.
What Are the Potential Financial Consequences of Air Ambulance Transport?
Patients should inquire about the potential financial consequences of air ambulance transport. This includes understanding the scope of coverage, potential balance billing, and any limitations or exclusions related to air ambulance services.
Are There Alternatives to Air Ambulance Services?
Patients should explore whether there are alternative transportation options available for their specific medical needs. In some cases, non-emergency ground transportation or specialized medical transport services may be viable alternatives to air ambulance services, potentially reducing costs.
By asking these and other relevant questions, patients can gain a better understanding of the air ambulance billing process and make more informed decisions regarding their healthcare and finances.
Conclusion
When it comes to air ambulance billing, transparency is paramount. By understanding the importance of air ambulance billing transparency, patients can navigate the complex world of medical billing with more confidence and control. With increased transparency, patients can budget and plan for the financial impact of air ambulance services, hold providers accountable for fair pricing, and avoid the hardships associated with surprise billing.
With a better understanding of the air ambulance billing process, including the role of insurance, common billing components, and the factors influencing costs, patients can advocate for themselves and make informed decisions about their medical and financial choices.
By being aware of billing practices, such as surprise billing and balance billing, patients can challenge unfair charges and seek resolution through appeals and consumer protection agencies. Additionally, by engaging in advocacy efforts, seeking support from relevant organizations, and campaigning for legislative changes, patients can drive improvements in air ambulance billing practices and protect the rights and financial well-being of themselves and future patients.